Having received several questions about fellow Welshman Aneurin Bevan's creation of a National Health Service in the United Kingdom, I am posting here chapter five of his book, "In Place of Fear". In it, Nye reflects on the opposition he dealt with, questions that arose and the early years of the Service. I think much of this commentary from 1952 is highly relevant to the questions facing the United States this presidential election year.
THE field in which the claims of individual commercialism come into most immediate conflict with reputable notions of social values is that of health. That is true both for curative and preventive medicine. The preventive health services of modern society fight the battle over a wider front and therefore less dramatically than is, the case with personal medicine.
Yet the victories won by preventive medicine are much the most important for mankind. This is so not only because it is obviously preferable to prevent suffering than to alleviate it. Preventive medicine, which is merely another way of saying health by collective action, builds up a system of social habits that constitute an indispensable part of what we mean by civilization. In this sphere values which are in essence Socialist challenge and win victory after victory against the assertions and practice of the competitive society.
Modern communities have been made tolerable by the behaviour patterns imposed upon them by the activities of the sanitary inspector and the medical officer of health. It is true, these rarely work out what they do in terms of Socialist philosophy; but that does not alter the fact that the whole significance of their contribution is its insistence that the claims of the individual shall subordinate themselves to social codes that have the collective well-being for their aim,
irrespective of the extent to which this frustrates individual greed.
It is only necessary to visit backward countries, or the backward parts of even the most advanced countries, to see what happens when this insistence is overborne. There, the small well-to-do classes furnish themselves with some of the machinery of good sanitation, such as a piped water supply from their own wells, and modem drainage and cesspools. Having satisfied their own needs, they fight strenuously against finding the money to pay for a good general system that would make the same conveniences available to everyone else.
The more advanced the country, the more its citizens insist on a pure water supply, on laws against careless methods of preparing and handling food, and against the making and advertising of harmful drugs. Powerful vested interests with profits at stake compel the public authorities to fight a sustained battle against the assumption that the pursuit of individual profit is the best way to serve the general good.
The same is true in relation to contagious diseases. These are kept at bay by the constant war society is waging in the form of collective action conducted by men and women who are paid fixed salaries. Neither payment by results nor the profit motive are relevant. It would be a fanatical supporter of the competitive society who asserted that the work done in the field of preventive medicine shows the enslavement of the individual to what has come to be described in the United States as 'statism', and is therefore to be deplored. The more likely retort is that all these are part of the very type of society I am opposing. That is true. But they do not flow from it. They have come in spite of it. They stem from a different order of values. They have established themselves and they are still winning their way by hard struggle. In claiming them, capitalism proudly displays medals won in the battles it has lost.
When we consider the great discoveries in medicine that have revolutionized surgery and the treatment of disease, the same pattern appears. They were made by dedicated men and women whose work was inspired by values that have nothing to do with the rapacious bustle of the stock exchange: Pasteur, Simpson, Jenner, Lister, Semelweiss, Fleming, Domagk, Roentgen - the list is endless. Few of these would have described themselves as Socialists, but they can hardly be considered representative types of the competitive society.
The same story is now being unfolded in the field of curative medicine. Here individual and collective action are joined in a series of dramatic battles. The collective principle asserts that the resources of medical skill and the apparatus of healing shall be placed at the disposal of the patient, without charge, when he or she needs them; that medical treatment and care should be a communal responsibility that they should be made available to rich and poor alike in accordance with medical need and by no other criteria. It claims that financial anxiety in time of sickness is a serious hindrance to recovery, apart from its unnecessary cruelty. It insists that no society can legitimately call itself civilized if a sick person is denied medical aid because of lack of means.
Preventable pain is a blot on any society. Much sickness and often permanent disability arise from failure to take early action, and this in its turn is due to high costs and the fear of the effects of heavy bills on the family. The records show that it is the mother in the average family who suffers most from the absence of a free health service. In trying to balance her domestic budget she puts her own needs last.
Society becomes more wholesome, more serene, and spiritually healthier, if it knows that its citizens have at the back of their consciousness the knowledge that not only themselves, but all their fellows, have access, when ill, to the best that medical skill can provide. But private charity and endowment, although inescapably essential at one time, cannot meet the cost of all this. If the job is to be done, the state must accept financial responsibility.
When I was engaged in formulating the main principles of the British Health Service, I had to give careful study to various proposals for financing it, and as this aspect of the scheme is a matter of anxious discussion in many other parts of the world, it may be useful if I set down the main considerations that guided my choice. In the first place, what was to be its financial relationship with national insurance; should the health service be on an insurance basis? I decided against this. It had always seemed to me that a personal contributory basis was peculiarly inappropriate to a national health service. There is, for example, the question of the qualifying period. That is to say, so many contributions for this benefit, and so many more for additional benefits, until enough contributions are eventually paid to qualify the contributor for the full range of benefits.In the case of health treatment this would give rise to endless anomalies, quite apart from the administrative jungle which would pe created. This is already the case in countries where people insure privately for operations as distinct from hospital or vice versa.
Whatever may be said for it in private insurance, it would be out of place in a national scheme. Imagine a patient lying in hospital after an operation and ruefully reflecting that if the operation had been delayed another month he would have qualified for the operation benefit. Limited benefits for limited contributions ignore the overriding consideration that the full range of health machinery must be there in any case, independent of the patient's right of free access to it. Where a patient claimed he could not afford treatment, an investigation would have to be made into his means, with all the personal humiliation and vexation involved. This scarcely provides the relaxed mental condition needed for a quick and full recovery. Of course there is always the right to refuse treatment to a person who cannot afford it. You can always 'pass by on the other side'. That may be sound economics. It could not be worse morals.
Some American friends tried hard to persuade me that one way out of the alleged dilemma of providing free health treatment for people able to afford to pay for it would be to 'fix an income limit below which treatment would be free while those above, must pay. This makes the worst of all worlds. It still involves proof, with disadvantages I have already described. In addition it is exposed to lying and cheating and all sorts of insidious nepotism.
And these are the least of its shortcomings. The really objectionable feature is the creation of a two-standard health service, one below and one above the salt. It is merely the old British Poor Law system over again. Even if the service given is the same in both categories there will always be the suspicion in the mind of the patient that it is not so, and this again is not a healthy mental state.
The essence of a satisfactory health service is that the rich and the poor are treated alike, that poverty is not a disability, and wealth is not advantaged.
Two ways of trying to meet the high cost of sickness are the group insurance and the attachment of medical benefits to the terms of employment. Group insurance is merely another way of bringing the advantages of collective action to the service of the individual. All the insurance company does is to assess the degree of risk in any particular field, work out the premium required from a given number of individuals to cover it, add administrative cost and dividends, and then sell the result to the public. They are purveyors of the law of averages. They convert economic continuity, which is a by-product of communal life, into a commodity, and it is then bought and sold like any other commodity.
What is really bought and sold is the group, for the elaborate actuarial tables worked out by the insurance company are nothing more than a description of the patterns of behaviour of that collectivity which is the subject of assessment for the time being. To this the company adds nothing but its own profits. This profit is therefore wholly gratuitous because it does not derive from the creation of anything. Group insurance is the most expensive, the least scientific, and the clumsiest way of mobilizing collective security for the individual good.
In many countries the law implicitly recognizes this because the insurance company is required to invest some, if not all, of its income in trustee stock, national bonds and debentures. In other words, the company must invest in those properties which bear the strongest imprint of continuous communal action. The nearer the investment approaches to those forms of property which are most characteristic of competitive capitalism, the less the element of collective security, and therefore the less desirable from the point of view of insurance. There never can be a clearer case of the private exploitation of a product publicly produced.
Where medical benefits are attached to employment as a term of the contract the situation is somewhat different. Here is an instance where the workers, as occupational groups, succeed in accomplishing what they have failed to do or not tried to do as enfranchised citizens. It has the one advantage that the employer in such a case will be less eager to lobby against legislation for a national health scheme. He may be inclined to support national proposals because these will make others share part of his burden. As a political tactic, therefore, occupational medical benefits have something to be said for them; and the workers enjoy some protection in the meantime while the national scheme is being held up.
But they are no substitute for a national scheme. An industrial basis is too narrow for the wide range of medical needs which should be met, both for the worker and for his family. The incidence of sickness varies from industry to industry and so do the rates of economic obsolescence and unemployment. We had experience of this in Britain where certain of the Approved Societies under the old National Health Insurance recruited a disproportionate number of members from industries with a high degree of sickness and accident rate and affected by serious industrial depression. The result was that these Approved Societies were compelled to curtail benefits to their members, while other societies with a different industrial composition were able to distribute the full benefits. That situation consequently helped the strong and hurt the weak.
There are two final objections to the methods I have been describing. They create a chaos of little or big projects, all aiming at the same end: assisting the individual in time of sickness. A whole network of strong points emerge, each with a vested interest in preventing a rational national scheme from being created. Thus to the property lobby is added the lobby of those who stand to lose under the national project. In the end they may have. to be bought out at great cost in time, effort and money.
The second objection is even more serious. These schemes all have for their aim the consumption of the apparatus of health. But they leave the creation of that apparatus without plan and central direction. In place of a rational relationship between all its parts, there arises a patch-quilt of local paternalisms. My experience has taught me that there is no worse enemy to the intelligent planning of a national health service, especially on the hospital side. Warm gushes of self-indulgent emotion are an unreliable source of driving power in the field of health organization. The benefactor tends also to become a petty tyrant, not only willing his cash, but sending his instructions along with it.
The other alternative is a flat rate compulsory contribution for all, covering the full range of health treatment, or a limited part of it. There is no advantage whatever in this. It is merely a form of poll tax with all its disagreeable features. It collects the same from the rich and the poor, and this is manifestly unjust. On no showing can it be called insurance.
One thing the community cannot do is insure against itself. What it can and must do is to set aside an agreed proportion of the national revenues for the creation and maintenance of the service it has pledged itself to provide. This is not so much insurance as a prudent policy of capital investment. There is a further objection to a universal contribution, and that is its wholly unnecessary administrative cost, - unless it is proposed to have graduated contributions for graduated benefits, and I have already pointed out the objections to that. Why should all have contribution cards if all are assumed to be insured? This merely leads to a colossal record office, employing scores of thousands of clerks solemnly restating in the most expensive manner what the law will already have said; namely, that all citizens are in the scheme.
The means of collecting the revenues for the health service are already in the possession of most modern states, and that is the normal system of taxation.
This was the course which commended itself to me and it is the basis of the finance of the British Health Service. Its revenues are provided by the Exchequer in the same way as other: forms of public expenditure. I am afraid this is not yet fully understood. Many people still think they pay for the National Health Service by way of their contribution to the National Insurance Scheme. The confusion arose because the new service sounded so much like the old National Health Insurance, and it was launched on the same date as the National Insurance Scheme. Some part of the misunderstanding was caused by the propaganda of the British Medical Association, which warned the people at one time that, although they would be paying their contributions, the Health Service would not be there to meet their needs. There was a certain irony about this, because when the time came for enrolment in the Health Service more than ninety per cent of the population hastened to get their names in, some under the impression, helped by the B.M.A. itself, that they had started paying for it. This gave me some quiet satisfaction.
One of the consequences of the universality of the British Health Service is the free treatment of foreign visitors. This has given rise to a great deal of criticism, most of it ill-informed and some of it deliberately mischievous. Why should people come to Britain and enjoy the benefits of the free Health Service when they do not subscribe to the national revenues? So the argument goes. No doubt a little of this objection is still based on the confusion about contributions to which I have referred. The fact is, of course, that visitors to Britain subscribe to the national revenues as soon as they start consuming certain commodities, drink and tobacco for example, and entertainment. They make no direct contribution to the cost of the Health Service any more than does a British citizen.
However, there are a number of more potent reasons why it would be unwise as well as mean to withhold the free service from the visitor to Britain. How do we distinguish a visitor from anybody else? Are British citizens to carry means of identification everywhere to prove that they are not visitors? For if the sheep are to be separated from the goats both must be classified. What began as an attempt to keep the Health Service for ourselves would end by being a nuisance to everybody. Happily, this is one of those occasions when generosity and convenience march together.
The cost of looking after the visitor who falls ill cannot amount to more than a negligible fraction of £399,000,000, the total cost of the Health Service. It is not difficult to arrive at an approximate estimate. All we have to do is look up the number of visitors to Great Britain during one year and assume they would make the same use of the Health Service as a similar number of Britishers. Divide the total cost of the Service by the population and you get the answer. I had the estimate taken out and it amounted to about £200,000 a year.Obviously this is an overestimate because people who go for holidays are not likely to need a doctor's attention as much as others. However, there it is. for what it is worth and you will see it does not justify the fuss that has been made about it.
The whole agitation has a nasty taste. Instead of rejoicing at the opportunity to practice a civilized principle, Conservatives have tried to exploit the most disreputable emotions in this among many other attempts to discredit socialized medicine.
Naturally when Britons go abroad they are incensed because they are not similarly treated if they need the attention of a doctor. But that also I am convinced will come when other nations follow our example and have health services of their own. When that happens we shall be able to work out schemes of reciprocity, and yet one more amenity will have been added to social intercourse. In the meantime let us keep in mind that, here, example is better than precept.
The National Health Service and the Welfare State have come to be used as interchangeable terms, and in the mouths of some people as terms of reproach. Why this is so it is not difficult to understand, if you view everything from the angle of a strictly individualistic competitive society. A free health service is pure Socialism and as such it is opposed to the hedonism of capitalist society. To call it something for nothing is absurd because everything has to be paid for in some way or another.
But it does mean that the Service is there to be used at the time you need it without payment anxieties. To put it another way, you provide, when you are well, a service that will be available if and when you fall ill. It is therefore an act of collective goodwill and public enterprise and not a commodity privately bought and sold. It takes away a whole segment of private enterprise and transfers it to the field of public administration, where it joins company with the preventive services and the rest of the communal agencies, by means of which the new society is being gradually articulated. Nor should we underestimate the size of the invasion we are making. In Britain there are more than 340,000 workers of various kinds engaged in the National Health Service. It costs about eight pounds per head of the population. (note 1) But a large proportion of this sum was being paid on private account before the Service started. It is impossible to estimate the exact amount. Some experts in this field go so far as to say they doubt whether there is any real net additional social cost, because of the innumerable harpies who battened on the sick and who are slowly being eliminated. Be that as it may, there is no doubting the magnitude of the enterprise. What is surprising is the smoothness of the transfer and the way it is settling down.
The prophets of disaster have been proved false, as they so often are when new and ambitious ventures are projected.
And now comes the question so frequently asked: do not all these free facilities invite abuse? Whenever I was asked that question I always answered: 'A prerequisite to a study of human behaviour is that human beings should first be allowed to behave.' When the Service started and the demands for spectacles, dental attention and drugs rocketed upwards the pessimists said : 'We told you so. The people cannot be trusted to use the Service prudently or intelligently. It is bad now but there is worse to come. Abuse will crowd on abuse until the whole scheme collapses.'
Those first few years of the Service were anxious years for those of us who had the central responsibility. We were anxious, not because we feared the principles of the Service were unsound, but in case they would not be given time to justify themselves. Faith as well as works is essential in the early years of a new enterprise.
The question uppermost in my mind at that time was whether a consistent pattern of behaviour would reveal itself among the millions using the Service, and how long would it take for this to emerge? Unless this happened fairly soon it would not be possible to put in reliable estimates for the Budget. The first few estimates for the Health Service seemed to justify the critics. Expenditure exceeded the estimates by large amounts, and Mr. Churchill with his usual lack of restraint plunged into the attack. In this he showed less insight than his colleagues, who watched his antics with increasing alarm. They knew the Service was already popular with the people. If the Service could be killed they wouldn't mind, but they would wish it done more stealthily and in such a fashion that they would not appear to have the responsibility.
Ordinary men and women were aware of what was happening. They knew from their own experience that a considerable proportion of the initial expenditure, especially on dentistry and spectacles, was the result of past neglect. When the first rush was over the demand would even out. And so it proved. Indeed, it was proved even beyond the expectations of those of us who had most faith in the Service.
It is not generally appreciated that after only one full year's experience of the Service I was able to put in an estimate which was firm and accurate. This was remarkable. It meant that in so short a space of time we were able to predict the pattern of behaviour of all the many millions of people who would be using the Service in a particular year. Whatever abuses there were, they were not on the increase. From that point on, any increased expenditure on the Service would come from its planned expansion and not from unpredictable use and abuse. We now knew the extent to which the people would use the existing facilities and what it would cost us. The ground was now firm under our feet. Such abuses as there were could be dealt with by progressive administrative pressure.(note 2)
Danger of abuse in the Health Service is always at the point where private commercialism impinges on the Service; where, for example, the optician is paid for the spectacles he himself prescribes, or the dentist gives an unnecessary filling for which he is paid. Abuse occurs where an attempt is made to marry the incompatible principles of private acquisitiveness with a public service. Does it therefore follow that the solution is to abandon the field to commercialism? Of course not. The solution is to decrease the dependence on private enterprise. The optical service is a case in point.
I have been told by ophthalmic surgeons that opticians prescribe spectacles sometimes when they are not really necessary. This, of course, the opticians hotly resent. The opticians protests would carry more weight if they were not also purveyors of spectacles. They thus make a profit out of their own advice and this tends to cast doubt on the advice itself.
This is an obvious defect in the British Health Service as it is now. I never intended it to remain. The present arrangements have always been regarded as temporary, to be replaced as follows. If the family doctor believes there may be something wrong with your eyes the best person to advise is the ophthalmic surgeon and not the ophthalmic optician. The latter is primarily concerned with those physical abnormalities that lead to defects of vision. The surgeon is interested in the physiological as well as the anatomical aspects. Under the revised scheme the patient would be sent to the surgeon, who would use the optician to give a reading of the eyes and so save his own time. Spectacles would then be provided only if the surgeon thought them necessary. Ophthalmic surgeons tell me that if this scheme were in operation fewer spectacles would be in use. And it would be to the advantage of the patient to be examined by the surgeon in the first instance, for he might find in the eyes evidence of morbidity of wider significance, and thus assist the patient to whatever other treatment might be necessary.
There are other and better ways of dealing with alleged abuses than by throwing in the sponge.
A free Health Service is a triumphant example of the superiority of collective action and public initiative applied to a segment of society where commercial principles are seen at their worst.
'The old system pays me better, so don't interfere.' Who would dare to put it so crudely? But it is as well to keep in mind that a public undertaking of this magnitude is big business. It touches trade and industry at a hundred sensitive points. A striking illustration of this was provided by our efforts to take proper care of the deaf. It had always seemed to me that this affliction had received too little attention. Deafness is a grievous handicap, worse some say even than blindness, though here we must speak with diffidence, because no one who has not suffered both can really judge. But this at least is agreed: deafness causes much personal suffering and industrial loss. The mechanical aids to deafness were often deficient, and always too expensive for all but a tiny section of those in need.
The way that seemed to offer the best chance of success was to bring the hearing specialist and the aural technicians into conference with each other, to see if a satisfactory aid could be devised, which could then be put into mass production and distributed through the hospitals. The effort met with outstanding success. By September 1951, one hundred and fifty-two thousand aids had been distributed and the users are enthusiastic about them.(note 3). They cost approximately one tenth of those on sale commercially. There is no reason why, after the home demand has been met, they should not prove the basis of a thriving export trade.
By bulk ordering of common essentials and cutting out unnecessary retail profit margins, as in the instance given, substantial economies can be made.
It is significant that few Conservatives mention this side of the Health Service. They are silent where economies could be made at the expense of profits. The possibilities of bulk ordering of whole ranges of hospital equipment and necessities, such as blankets and linen, were realized early in the development of the scheme. In order to extend the advantages of this over a wider field of public expenditure the Supply Department of the Ministry of Health was made responsible for the medical needs of the Armed Forces. When all these are fully integrated, the result should make a significant impact on the private sector of the industries affected. The manufacturers will be afforded a reliable estimate of the requirements of the public authorities and can adjust their production flows accordingly, while improved specifications should improve quality and reduce cost.
But the hardest task for any public representative charged with the duty of making a free Health Service available to the community is overcoming the fears, real and imaginary, of the medical profession. His task is to reconcile the general public interest with their sectional claims. No pressure groups are more highly organized in Britain than the professions, and among these the medical professions are the strongest.
I was anxious to ensure that the general practitioner should be able to earn a reasonable living without having to aim at a register which would be too large to admit of good doctoring. To accomplish this I suggested a graduated system of capitation payments which would be highest in the medium ranges and lower in the higher. This would have discouraged big lists by lessening the financial inducement. The B.M.A. refused this, although now I am told they are ready to reopen the question. Had they agreed at the time the position of doctors in the overdoctored areas of the country would have been made easier as redistribution over the country as a whole gradually took place.
I have a warm spot for the general practitioner despite his tempestuousness. There is a sound case for providing a little more money to help the doctor with a medium list who wants to make a decent living and yet be a good doctor. The injection of several million pounds here would refresh the Service at its most vulnerable point: that is, the family. doctor relationship. The family doctor is in many ways the most important person in the Service. He comes into the most immediate and continuous touch with the members of the community. He is also the gateway to all the other branches of the Service. If more is required than he can provide, it is he who puts the patient in touch with the specialist services.(note 4)
He is also the most highly individualistic member of the medical world. As soon as he leaves medicine he seems to think in slogans. These are shot through with political animus of the most violent description - usually Conservative. I speak here primarily of the British Medical Association. The Medical Practitioners' Union on the other hand is a progressive body, affiliated to the Trades Union Congress and more up-to-date in its views. But it was with the B.M.A. I had to negotiate. I usually met its representatives when they had come hot from a conference at which the wildest speeches had been made, frequently by the very men who then had to try to come to terms with the people they had been so immoderately denouncing.
I enjoyed the challenge. My trade union experience had taught me to distinguish between the atmosphere of the mass demonstration and the quite different mood of the negotiating table. I was therefore able to discount a great deal of what had been said from the rostrum. Also it was easy for me to enable them to win victories, for they had usually worked themselves up into a fever of protest against proposals which had never been made. Thus they would 'never be made into civil servants'. (note 5). As I never intended they should, I was able to concede the point without difficulty.
Then there must be 'free choice of doctor'. I myself was most anxious to insist on this, for I saw in it one of the most important safeguards for the public. The right of the patient to leave his doctor and choose another whenever he liked had a double edge that the B.M.A. spokesmen did not fully appreciate until later. Then there was the demand for full rights of free expression of opinion, both about the Health Service and anything else. To this again I was most ready to respond, as it had never occurred to me that anything otherwise had been intended.
And so it went on from one blown-out slogan to another. Indeed, I warned the leaders of the profession that they were making a fundamental mistake in strategy. They were mobilizing their forces to fight a battle that was never likely to begin. When later I was able to make a considered statement in Parliament giving a solemn undertaking to abide by principles that were my own from the very start, the B.M.A. found its forces leaving the field just when the crucial stage in the struggle was reached.
In speaking of the medical profession I must not be thought to be speaking at the same time of the individual men and women who make it up: In their case, as in so many others, the psychology of the profession as a whole is not the sum of its individual parts. Indeed, this seems to be much more the case with doctors than with other social groups. In my dealings with them I was soon made aware of two curious streams of thought. In the first place the general public has no great faith in the medical profession considered as a collectivity, which in no way interferes with a warm attachment between individual doctors and patients. Statesmen anxious to establish a free Health Service should keep that in mind. In a conflict between the profession and the general public the latter will always win if they are courageously led. The pretensions of the medical profession as a special social group are resented by the' generality of citizens. They savour too much of caste and privilege. The practice of medicine is still so much more an art than a science that its practitioners do not seem to the laity to be justified in the atmosphere with which they are apt to surround themselves. There is a good deal of hit and miss about general medicine. It is a profession where exact measurement is not easy and the absence of it opens the mind to endless conjecture as to the efficacy of this or that form of treatment.
The doctors themselves insist on this element of unpredictability in the response of individual patients to various forms of treatment. They affirm that individuals differ so much that there is always a high subjective content in the practice of medicine. This arises in a variety of ways; in the medical history of the patient, his work, his relations with his family and with the society of which he is a member. All these apparently have to be taken into account in diagnosis and treatment. This we accept, and indeed it is fairly obvious. What is not so obvious is that the average doctor is equipped by his general education and by temperament to make an assessment of so many imponderables. He requires for this delicate task imaginative sympathy, sensitivity, and a1iberal education; and these are not so widespread in the profession as many of us would like to see. That there are such gifted persons we know, and they are of infinite benefit to suffering mankind. But in this field, with its margin of error, the quack, the charlatan and the ill-equipped also flourish, and there are few tests the layman can apply to safeguard himself.
In my discussions with many of the best members of the medical professions in Britain they have individually always been ready to admit this with true scientific humility. But the margin of possible error which is part of their daily experience does not free them from what can only be described as a collective arrogance. This is accompanied by waves of something approaching mass hysteria whenever proposals affecting their profession are advanced. We saw it in Britain, we have seen it in Australia and, New Zealand, and now it appears to have the medical profession of the United States in its grip.
In dealing with the medical profession it is wise to make a distinction between three main causes of opposition to the establishment of a free National Health Service. There is the opposition which springs from political opinion as such. This is part of the general opposition of Conservative ideas, and it is strong in the medical profession, though the expression of it tends to be supercharged with the emotions borrowed from other fears and ambitions. Second, there is the defence of professional status and material reward. The latter, of course, they share with other pressure groups. Then, thirdly, there is the opposition which springs from the fear that lay interference might affect academic freedom and come between the doctor and his patient. The third group is the most legitimate and will unite all the members of the medical world, from the self-seeking to the truly idealistic. Any health service which hopes to win the consent of the doctors must allay these fears. The fear of state interference in academic matters is very strong in the Western world, although it tends to ignore the power that patronage already has to influence the pattern of medical investigation. Nevertheless, entitlement to advancement on grounds of merit alone, free from any tinge of political nepotism, must be jealously guarded by any self-respecting profession. Nor should less informed opinion be allowed to influence the medical curriculum. Here there is no substitute for the refreshment of renovating influences within the profession itself. Freedom of discussion and a readiness to add to, and receive from, the corpus of accepted knowledge, are the only ways we have yet discovered to safeguard what we have gained, and to open ways to new discoveries.(note 6) The medical profession is cautious, some say unduly so, in accepting new ideas. This has been impressed upon me over and over again by those who claim to have discovered methods of treatment and cure other than those normally practised by the profession. On the other hand, it is my experience that unorthodox practitioners are often the worst quacks, and when offered a fair hearing, unwilling to expose themselves to the disciplines of controlled experiment and verification. As a general rule they advance testimony in place of evidence and credibility in place of informed conviction.
There is no alternative to self-government by the medical profession in all matters affecting the content of its academic life, although there is every justification for lay co-operation in the economy in which that is carried out. The distinction between the two is real. It is for the community to provide the apparatus of medicine for the doctor. It is for him to use it freely in accordance with the standards of his profession and the requirements of his oath.
This is also the case with respect to the relations between the doctor and his patient. A great deal of nonsense has been talked about this. There never has been any danger that socialized medicine would destroy the privacy of doctor-patient relationship. Such a danger would indeed rupture a health service from the start. The privacy rightly accorded a patient under a health service is much more than is often the case in, for example, private insurance. The consulting room is inviolable and no sensible person would have it otherwise.
The defects in the Health Service that have been brought to light by practical experience lie in quite other directions. Although it is essential to retain parliamentary accountability for the Service, the appointment of members of the various administrative bodies should not involve the Minister of Health. No danger of nepotism arises, as no salaries are attached to the appointments, but election is a better principle than selection. No Minister can feel satisfied that he is making the right selection over so wide a field. The difficulty of applying the principle of election, rather than selection, arises from the fact that no electoral constituency corresponds with the functional requirements of the Service. This is particularly so in the case of hospital organization. Hospitals are grouped in such a way that most, if not all, the different medical specialties are to be found within a given area.
A solution might be found if the reorganization of local government is sufficiently fundamental to allow the administration of the hospitals to be entrusted to the revised units of local government. But no local finances should be levied, for this would once more give rise to frontier problems; and the essential unity of the Service would be destroyed.(note 7)
Another defect of the Service, which was seen from the beginning, is the existence of pay beds in hospitals. The reason why this was tolerated at all was because it was put to me by the representatives of the royal colleges that in the absence of pay-bed sections in the hospitals the specialists would resort in greater measure to nursing homes. As the full range of medical facilities are available only in the hospitals as a general rule, the specialists should be there, on the spot, as much as possible. The argument is sound, but there can be no doubt that the privilege has been abused. Pay beds are a profitable source of income to the specialists, and there is therefore a disposition to prefer patients who can afford them at the expense of others on the hospital waiting lists. The number of pay beds should be reduced until in course of time they are abolished, unless the abuse of them can be better controlled. The number of 'amenity beds' should be increased. These are beds for which the patient pays a small sum for privacy alone, all the other services being free. These changes would mean a loss of revenue to the National Health Service, but they would cut out a commercial practice which undermines the principle of equality of treatment that is fundamental to the whole conception of the scheme.
Doubtless other defects can be found and further improvements made. What emerges, however, in the final count, is the massive contribution the British Health Service makes to the equipment of a civilized society. It has now become a part of the texture of our national life. No political party would survive that tried to destroy it.
Since this chapter was written, new legislation on the National Health Service has been announced. It confirms our worst fears. If they are carried out the proposals will mutilate the Service in many of its most important activities. There is, however ample evidence that the British people are reacting sharply against them. This sustains my contention that no government that attempts to destroy the Health Service can hope to command the support of the British people. The great argument about priorities is joined and from it a free Health Service is bound to emerge triumphant.
NOTE 1
In estimating the cost of the Service it is necessary to consider the range of its operations and the facilities it provides. It covers all forms of treatment, mental as well as physical. For the first time these are integrated. Mental ill health is no longer regarded as belonging to a world of its own. I consider this to be one of the outstanding features of the British Health Service. The separation of mental from physical treatment is a survival from primitive conceptions and is a source of endless cruelty and neglect. The mentally ill are looked upon as people who have stepped outside normal intercourse and this fact itself often accentuates and perpetuates the trouble. If at the early stages of mental disturbance the patient is able to get advice, not at a mental institution, but by a mental specialist in a general hospital, then subsequent degeneration can frequently be prevented. The very fact that they go amongst the general streams of patients for consultation and are not hived off on their own is itself a source of helpful self-confidence.
Then there is the provision that enables mental patients to enter mental homes voluntarily and leave when they like. In 1931 voluntary admission represented only 7 per cent of the total admissions, whereas by 1949 the proportion had risen to 63 per cent.
NOTE 2
Drugs are consumed in too large quantities. Few doctors would disagree with that statement. It was so before the Health Service. Indeed, excessive consumption can be described as one of the diseases of modem civilization. The solution is firmness by the doctor and education of the patient. If there is abuse in this side of the Service the fault lies primarily with the doctor. The chemist cannot dispense what the doctor does not prescribe. Some doctors argue that if they do not give the patient something to take he will leave them and go to another doctor. This is one of the instances of 'free choice of doctor' which, according to the campaign by the B.M.A. when the Service was being formed, was not supposed to exist.
A great deal can be done by a more intensive education of the general population. This would improve the health of the population as well as reduce the burden on the Health Service. Much more imaginative use could be made of the BBC and of television to acquaint the people with the consequences of too much drug-taking. It would also have an appreciable effect on the number of patients attending at the doctors' surgeries.
Already steps had been taken when I was at the Ministry of Health to attack the problem from another and even more promising angle. That was to forbid the consumption in the service of drugs which are generally advertised. These are usually more expensive and often no better, indeed frequently inferior, to the drugs contained on the official lists and the recognized Formulary. The effect of this is threefold. It reduces the pressure of the credulous patient on the doctor when the former demands something he has seen advertised for its miraculous properties. Second, it discourages the production and advertising of these concoctions. Thirdly, it will substantially reduce the cost of prescriptions with the Health Service. These are the answers to whatever abuses may exist on the pharmaceutical side of the British Health Service.
NOTE 3
Number of Hearing Aids - cumulative figures:
New Patients
Up to December, 1948 7,51 1
Up to December, 1949 48,734
Up to December, 1950 114,835
Up to September, 1951 152,000
NOTE 4
As time goes on it is hoped that general practitioners will find it better to work in groups, whether at a health centre or otherwise. There are advantages in this. The work could be shared between them so as to reduce the strain on the individual doctor. Night calls are an obvious example. Group consultation would put the knowledge and experience of all at the disposal of each, and the natural desire to stand well in the eyes of his fellow craftsmen would tend to raise and maintain standards.
There is still a question-mark against health centres. There is no doubt about their desirability. But there should be a limit to what should be attempted in them. It would be an expensive duplication if they developed into rivals of the out-patient departments of general hospitals. Here further experience is necessary before final decisions are made.
NOTE 5
The fear that the Health Service would result in an army of civil servants was got over by establishing a contractual relationship, not with the Minister of Health but with the boards of governors of teaching hospitals, the regional hospital boards and, in the case of the family doctors, chemists and opticians, with the local executive councils. Thus central responsibility for a national service is reconciled with the principle of dispersed supervision. This is exercised through the medium of voluntary workers. It is not sufficiently understood that all the members of the boards, management committees of hospitals, and members of executive councils serve voluntarily. This is partly responsible for the low administrative cost of the Service.
The separate expenses of the bodies engaged in the administration of the British National Health Service amount to about 3 per cent of the total sum spent. 60 per cent of the expenditure of the hospitals lies outside the jurisdiction of the hospital authorities. Wages and salaries are fixed by national agreement by means of Whitley awards. The area of expenditure left to the hospital authorities within which they can exercise direct economy is, therefore, about 40 per cent of the total.
The local executive councils are composed of representatives of the county councils and county boroughs, committees of the three professions, medical, chemical and optical, along with persons appointed direct by the Minister of Health. This body is responsible for the administration and discipline of the three services. It is therefore the strongest line of defence against abuse, and the body in most immediate contact with members of the general public. On the whole it is working well, except that the county area tends to be too far from the individual citizen. But that must wait upon a reorganization of local government.
NOTE 6
It is one of the distinct advantages of a national service that the use of improved health techniques and new discoveries of treatment are immediately generalized throughout the service. This is an advance on the past where superior methods worked their way slowly down from the few institutions and individuals that could afford them until long afterwards they reached - if they ever did - the poorer members of the community.
The question may be asked, what facilities are made available for research in this set-up? There is first the Medical Research Council, a body which has been in existence for many years and is under the supervision of a committee of the Privy Council. Some contend that the Medical Research Council should be brought within the administration of the Health Service. I am inclined to support this view. British science has always suffered from the distance which separates 'pure' from applied science. It is this which is partly responsible for the curious phenomenon, referred to on many occasions, that in Britain original discoveries are made which are not followed up in the practical field. Antibiotics is an example.
A closer relationship should be established between the potential user of the results of research and the research itself. The practical and the theoretical are two aspects of the same activity. Their separation is a hangover from the days of cloistered learning.
Research goes on in many of our hospitals all the lime, as well as in the private laboratories of commercial companies. More money is now available than at any time in the history of medicine. Most of the teaching hospitals have large sums at their disposal for this purpose. Their endowments were not touched when they were taken over into the Health Service.
But it is not only necessary to discover new knowledge and improve on old techniques. We must also see to it that useful aptitude and skills are not lost. Every war produces its tragic host of maimed, crippled and paralysed. Each time a pool of exceptional knowledge is accumulated to cope with the problem. As the number of patients declines with the passage of time, this contracts, is in danger of being lost and further improvements not pursued with the same drive. The department of the Ministry of Pensions which provides artificial limbs, eyes, ingenious chairs and cars, expanded at the end of the war and would have contracted after the normal pattern. But the civilian population also has its casualties, in the total sometimes as great as those in the services. Here the National Health Service performs an invaluable service. It maintains the pool of skill accumulated by the war and places it at the disposal of the civilian population. The technicians are not dispersed but are kept in continuous employment. If war comes again they will be there, ready immediately to mitigate disability and suffering to the limits of human ingenuity.
When the National Health Service started and free artificial limbs were made available, it was a revelation to witness the condition of the old ones left behind. It was a grim reminder of the extent to which the crippled poor had been neglected.
Number of artificial limbs and surgical appliances, issued from July 1948 to 31 August, 1951:
New Boots 112,556
Leg Instruments 69,987
Trusses 61,852
Belts 388,172
Wigs 28,617
Spinal Supports 80,652
Artificial Legs 30,002
Artificial Arms 6,003
Motor Propelled Tricycles 4,718
Hand Propelled Tricycles 3,190
Other Types of Chairs 11,290
NOTE 7
Local authorities are notoriously unwilling to delegate any of their functions or responsibilities to others. If hospital administration is entrusted to them they must be prepared to give generous support to the staff committees already established in the hospitals. The problem of how to associate the workers in the making of policy and in affairs of day-today administration is as real in the hospital world as it is elsewhere.
By revised units of local government is not meant regional local government areas. These would not be local government units in any proper sense of the term.
Full story...
Monday, July 28, 2008
In Place of Fear: A Free Health Service
Posted by
Jaz
at
11:02 AM
1 comments
![]()
Labels:
commentary
Social: DiggIt!
Del.icio.us
Technorati
Friday, July 25, 2008
If The Cure for Health Costs is Competition, the Prescription is Transparency

All too often in conversation about universal health care coverage, universal access, or the rising cost of health care, many American people I talk to fall back on the trusty free market response: a free market with healthy competition produces value.
I don't dispute this, having been born and raised in a much more left-leaning UK economy that doles out social welfare money like there's no tomorrow, I'm happy and excited to be part of the US economy, I've done well for myself here and probably far better than I would have if I'd stayed at home.
My first argument is always that it's the job of any government to provide health care for it's citizens. Aneurin Bevan put it best, I won't try to rewrite it, but it seems embarrassing to me that the US government can't provide health care for all. They already pay for about 40% of all health care in the country, which puts a big dent in the knee-jerk "we don't want government choosing our health care" you hear all too often in the US, fact is, they already do for half of all health care provided in the US. However, unlike Britain's National Health Service, which employs the doctors, in the US the government is merely a payer, they pay the bills, but you have to shop around for a private provider. Military care aside, the government doesn't employ health care providers.
That leaves us with a quasi free market economy where people are free to shop and choose their provider, shop and choose their insurance company, and generally exploit free market capitalism to restrain health care costs. Value is derived from competitive choice.
So wherein lies the rub?
First and foremost, a lot of people do not have any choice. They see the doctor nearest them that is a member of their health plan. They go to the hospital where their doctor has privileges, or they go to the only hospital in their vicinity. They may only have one option for their health care insurance, if they have receive insurance from their employer. And of course, yes, they might not even have health insurance.
I was once an uninsured middle class American. When I first came to the US myself and my wife were uninsured for a good five years. My (American) wife wanted me to buy health insurance, which I could never fully understand. As a Brit I knew that Americans were often subject to huge medical bills, but as I was told it the insurance I would get would not cover major medical expenses, just the routine stuff, and as I calculated it we were spending about $500 a year on health care.
When I finally caved in and acquired health care for us through a Small Business Association (I was self-employed at the time, late 1990s) I paid about $1600 a quarter - $6400 a year - to cover $500 worth of consuming. I still don't get it.
The argument you'll get from health care economists is that us young, healthy people need to pay into the pool to balance out the cost of caring for older, sicker people.
I'm not at all averse to that, in fact I advocate for it. It's called socialised medicine and I'm 100% behind it, I'd just prefer to pay my government in the form of taxes than private HMO companies in the form of padding their CEO profits. At least that way maybe we could cover everyone for 18% of GDP instead of 60-70% for 18% of GDP.
I'd prefer it if everyone was covered for 10% of GDP, but that's not likely here. Most developed countries provide health care for all for much less than 10% of GDP, yet in the US, which is currently spending about 18% of GDP on health care, even spending double doesn't cover everyone.
Makes sense?
Nope.
Moving on, for those people who *are* covered through their job, they are basically getting $9,312 in health care coupons on top of their salary. The average cost of providing health insurance in 2008 is over $9,000. If the median income is $36,835, and it is, then that means the average person with average health care coverage makes on average a quarter of their compensation via invisible health care money.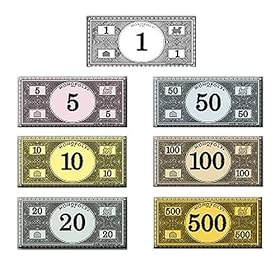
25% of your compensation is health care Monopoly money. What you do?
I'd spend it.
So we have an expectation from American workers that they will receive health care coverage from their employer, we have an expectation from HMOs to turn a profit, and we have a bunch of people with what are, for all practical purposes, coupons for free health care with little to no accountability for what the health care consumed actually costs.
If we expect competition to drive down costs, we need to know what things cost. Competition in the footwear industry would not be possible if we did not know how much shoes cost. We know what cars cost, we know what cheese costs, we know what haircuts cost, and we make decisions based, in varying degrees, on cost.
FREE MARKET COMPETITION CANNOT EXIST WITHOUT TRANSPARENT PRICING.
Why do we even have to use the word transparent? We don't call supermarkets transparent. Of course they put their prices on their products, how else could we stimulate competition? Houses have prices. Vacations have prices. Colleges have prices.
Enough already. Either we have universal coverage through taxation (please do not mandate me to buy health care from a private, shareholder corporation) or we have a free market. The US system is no less paternalistic than anything in Europe, the only real difference is there are people profiting from the money as it flows uphill.
We cannot have a free market without price conscious shoppers.
Can we?
You tell me what you think.
Full story...
Posted by
Jaz
at
10:08 AM
5
comments
![]()
Labels:
commentary,
insurance
Social: DiggIt!
Del.icio.us
Technorati
Monday, July 14, 2008
NHS Maternity Report
The Guardian has an article on the recent review of Britain's maternity services. Well worth the read.
Perhaps even more interesting is the letters to the editor published yesterday, including one that references an 1845 health care quality reporting law, which led me to find this outcomes report from the 1850s. For the full report: Towards better births - A review of maternity services in England (pdf 1262kb) (opens new window)
Full story...
Posted by
Jaz
at
12:22 PM
0
comments
![]()
Labels:
commentary
Social: DiggIt!
Del.icio.us
Technorati
Tuesday, July 8, 2008
New York Acquired Infections Report... For Dummies
I've been following the progress of New York State's Hospital Acquired Infection reporting initiative since the law was first passed. NY was given a year to pilot the reporting, and to provide a public report in aggregate the first year, moving to hospital-specific reporting the next.
I've read the report, and while it's certainly a great move forward for transparency it's hardly easy to read. Weighing in at 115 glorious pages, it makes it hard to figure out exactly what it's saying. Therefore, I give you NY HAI For Dummies!
The report covers three topics: central line-associated blood stream infections in critical care unit patients, and surgical site infections associated with colon and coronary artery bypass graft procedures. CABG reports on both the chest incision and the secondary (leg) incision. Further, patients are given a risk factor ranging from zero to four, four implying plenty of risk for infection (long surgery time, dirty incision site etc.)
For each topic and risk factor, NY has an opportunity to be statistically significantly better, the same, or worse than (older) national rates provided by the CDC. One huge caveat: the "national rates" against which NY is compared are from data spanning 1992 to 2004, so I'm not sure they honestly comparable, but at this point in time it's all anyone's got.Colon Procedure Surgical Site Infections
SSI Risk 0: 4.5% Same
SSI Risk 1: 6.3% Worse
SSI Risk 2: 7.6% Same
SSI Risk 3: 9.4% Same
1,082 reported infections of which MRSA (the "superbug") accounted for 110 cases or 10.2% and was the third most occurring organism.Coronary Artery Bypass Graft with Chest and Donor Site Incisions
Leg SSI Risk 0: 0.0% Same
Leg SSI Risk 1: 0.8% Better
Leg SSI Risk 2: 1.6% Better
Leg SSI Risk 3: 0.0% Same
Chest SSI Risk 0: 0.0% Same
Chest SSI Risk 1: 2.2% Same
Chest SSI Risk 2: 3.2% Same
Chest SSI Risk 3: 5.3% SameCoronary Artery Bypass Graft with Chest Incision Only
Chest SSI Risk 0: 20% (1 of 5 procedures) Same
Chest SSI Risk 1: 0.9% Better
Chest SSI Risk 2 & 3: 4.0% Same
503 total infections reported, of which MRSA accounted for 76 or 15.1%.Central Line-Associated Blood Stream Infection (CLABSI) Rates
Coronary ICU: 2.2 Better
Cardiothoracic Surgical ICU: 2.0 Same
Medical ICU: 3.2 Same
Med Surg - Major Teaching: 2.4 Same
Med Surg - All others: 2.3 Same
Pediatric ICU: 4.0 Better
Neurosurgical ICU: 3.1 Same
Surgical ICU: 3.7 Worse
A central line infection rate is calculated by dividing the number of actual infections by the length in days all the lines are in and multiplying by 1,000. So if a patient has a central line inserted for 24 hours that's one "surgical line day".
Interestingly, when the report compares upstate NY to New York City, it stands out that NYC is the same across the board, whereas upstate stands out as being the offenders bringing the state average worse. I help out a little with the CLAB infection collaborative initiative run by UHF and GNYHA over on Jeny, so I know there's a bunch of hospitals more city than not who are actively working on reducing CLAB infections. I have no idea if that's attributable or not, but sure is interesting.
(Edit: on second reading I noticed on p.39 the author references the collaborative as a potential factor in the lower numbers.)
1,348 infections reported, MRSA counting 83, or 6.2%
That's the easy-to-read and way-too-simplified summary, there's a wealth more data in the report including CLAB bundle compliance and NICU numbers and much more, I urge you to download it. If nothing else, let's show the Department of Health we're interested in their reports.
Full story...
Posted by
Jaz
at
6:52 PM
3
comments
![]()
Labels:
commentary,
public reporting
Social: DiggIt!
Del.icio.us
Technorati
Disclosures and Disclaimers
Disclosures
My employer is compensated through funding to provide analytical research, technology solutions, and Web-based public and private health care performance reports by the State of New York, the State of Illinois, the Centers for Medicare & Medicaid Services, the Agency for Healthcare Research and Quality, the Commonwealth Fund and Bridges to Excellence. I am not being compensated by any of these organisations to create articles for or make edits to this Web site or any other medium; and all posts authored by me are as an individual and do not represent my employer or the agencies I work for.



